Evaluation of Virtual Wards in Greater Manchester
What are we trying to do?
We are undertaking an independent evaluation of the Virtual Wards service being implemented across Greater Manchester. We aim to understand how Virtual Wards are organised and delivered across GM, explore patient, carer, and staff experiences of receiving or providing care on Virtual Wards, and assess whether Virtual Wards provide an effective, safe, efficient, and equitable approach to delivering care.
Why is this important?
The health and care systems across England was challenged with implementing a Virtual Wards service by December 2023. ARC-GM researchers Prof. Emma Vardy and Dr Gill Norman co-authored a Position Statement published by the British Geriatrics Society (BGS) about Virtual Wards in relation to older people.
The BGS definition of a Virtual Ward is
“a time-limited service enabling people who have an acute condition or exacerbation of a chronic condition requiring hospital-level care to receive this care in the place they call home, either as an alternative to hospital admission or by facilitating an earlier discharge from hospital.”
NHS England describes Virtual Wards as
“allowing patients to get the care they need at home safely and conveniently, rather than being in hospital” (see here for more information)."
Crucially, Virtual Wards deliver a variable combination of remote monitoring and face-to-face treatment in the person’s normal place of residence (at home or in a care home). Virtual Wards supported by NHS England funding will include an element of technology to help staff to monitor patient physiological observations remotely.
A recent rapid evidence synthesis (RES) published in Age & Ageing by Prof. Vardy and Dr Norman from ARC-GM, indicated that there is limited evidence of clinical effectiveness of Virtual Wards. Importantly the publication includes a practical synopsis of terminology used in clinical practice in relation to Virtual Wards, hospital at home and remote monitoring.
Our planned evaluation of Virtual Wards in Greater Manchester offers us an opportunity to work closely with our key stakeholders to inform regional and national decision making.
Prior to this study, we did a systematic review of technology-enabled innovations of Virtual Wards and hospital at home. The analyses, which included 69 studies (38 randomised and 31 non-randomised) and described 63 interventions, found that none of the technology-enabled care at home models explored put people at higher risk of readmission compared with hospital-based care. There also appeared to be no additional risk of mortality due to use of technology-enabled at home models. It was unclear whether inpatient-level care at home using higher levels of technology provided additional benefits.
How are we doing it?
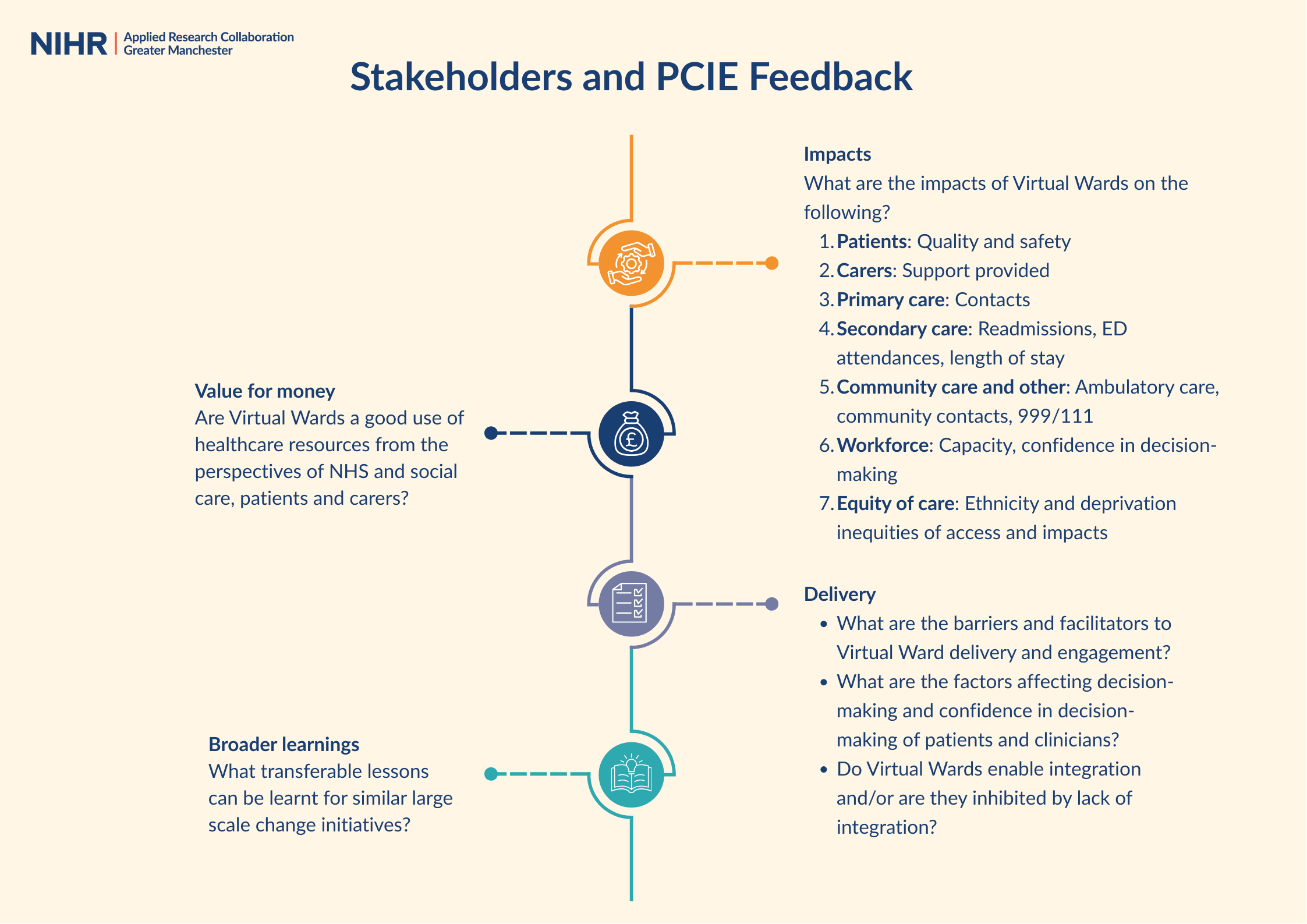
We are using a mixed-methods approach to address priority questions identified by GM stakeholders, including public contributors. The broad areas of interest include:
- Implementation and delivery of the Virtual Wards service;
- Referral and admissions processes;
- Organisation of care;
- Experiences of patients and carers in receipt of the service;
- Experiences of staff providing the service.
The study consists of three key work packages:
Work Package 1: Understanding how Virtual Wards are being implemented and delivered in GM
This package involves:
- Qualitative interviews with Virtual Ward service and implementation leads to explore topics such as the key components of the Virtual Wards models adopted, how the Virtual Wards service is integrated at the system level, and the processes for referral, eligibility assessment, and admission.
- Analysis of Virtual Wards data held by the NHS to understand the extent of Virtual Wards activity generated across GM, how it has changed over time, and to inform qualitative interviews. This includes summarising Virtual Wards capacity and activity by locality, day of the week, care pathway, step-up versus step-down models of care, and patient demographics.
Work Package 2: Understanding patient, carer, and staff experiences of receiving and providing care on Virtual Wards in GM
We will collect in-depth qualitative data from up to four NHS sites to explore:
- Staff, patient, and carer experiences through interviews.
- How different patients and providers experience Virtual Wards and what being on a Virtual Ward is like through observations in Virtual Ward settings and patients’ homes.
Work Package 3: Assessing clinical, cost and system outcomes of Virtual Wards in GM
We will assess the outcomes of Virtual Wards using quantitative data for all 10 GM boroughs, focusing on:
- Safety and clinical effectiveness of Virtual Ward care, and any differences by types of Virtual Ward care.
- Assessment of cost.
- Impact of the Virtual Wards care model on system-level healthcare utilisation and waiting times.
Public and Community Involvement and Engagement
The Virtual Wards evaluation was developed and is supported by ongoing public involvement work. The research team have collaborated with the ARC-GM PCIE Theme and the NIHR Greater Manchester Patient Safety Research Collaboration to do this, including members of the ARC-GM PCIE Panel and wider community groups.
At the start of the project, public members were consulted on what the broad areas of focus should be. Over the course of the project, materials were developed which summarise the perspectives of several groups on Virtual Wards.
Who are we working with?
- Health Innovation Manchester
- The Greater Manchester Integrated Care Partnership
- The Greater Manchester Virtual Ward Programme Board
- NIHR Greater Manchester Patient Safety Research Collaboration
Contact information:

Programme Manager
Dr Ross Atkinson
ross.atkinson@manchester.ac.uk