Collaborative Interventions for Circulation and Depression (COINCIDE)
Please see the downloable resources section of this web page to access the COINCIDE training manuals, these can be freely donwloaded.
Background
Significant gains have been made in primary care over recent years to improve access to and quality of depression care, with one promising intervention being ‘collaborative care’, a complex intervention which involves the use of a non-medical case manager – e.g. a Psychological Wellbeing Practitioner (PWP) or a nurse – working in conjunction with the patient’s doctor, often with the support and supervision of a mental health specialist (normally a psychiatrist or psychologist). Between 2008-13, NIHR CLAHRC Greater Manchester tested a collaborative care approach known as Collaborative Care for Circulation and Depression (COINCIDE) in the NHS, which involved a clinical trial across the north-west in 36 GP surgeries using trained Psychological Wellbeing Practitioners (PWPs) and practice nurses to deliver the COINCIDE intervention, based on a collaborative care model. Most collaborative care trials have previously been conducted in the United States; the Clinical Effectiveness of Collaborative Care for Depression in UK Primary Care Trial (CADET) was an important first step to showing collaborative care can work in the NHS, but it did not exclusively look at treatment of people with long term conditions or multi-morbidity. Read this research paper, published in the British Medical Journal (BMJ), to find out more about the first test of collaborative care in the NHS.
About the COINCIDE trial
COINCIDE was run as a ‘pragmatic’ trial in that it tested collaborative care in real world settings, using Improved Access to Psychological Therapy (IAPT) services and practice nurses. It aimed to show reductions in depression and also other patient reported outcomes such as quality of life and self-management behaviour.
- Key points on the rationale aims and design of COINCIDE
-
CADET trial showed benefits of collaborative care can translate to NHS;
-
But uncertainty about the effectiveness of collaborative care for managing depression in LTCs (including multi-morbidity) in settings that resemble routine care;
-
COINCIDE aimed to test the (cost) effectiveness of an integrated collaborative care model for People with depression and diabetes/coronary heart disease;
-
Interventions were delivered by existing providers (i.e. IAPT and practice nurses);
-
Patients had freedom to choose a variety of psychological treatments and/or medication.
Trial design
-
Pragmatic cluster-randomised controlled trial conducted in 36 GP surgeries across North West England;
-
Compared integrated collaborative care with usual care;
-
Primary outcome – severity of depression at 4/6 months using the SCL-D13;
-
Secondary outcomes – disease specific QOL, anxiety (GAD-7), QOL (WHOQOL-BREF), self-efficacy, patient ‘centred-ness’ (PACIC) patient self-management behaviour (heiq), patient satisfaction (CSQ-8), social support (ENRICHD), healthcare utilisation and health utilities (EQ-5D).
For further information about the rationale and design of COINCIDE, please read the Trial papers published in Trial Journal in August 2012 and May 2013
COINCIDE Care Model
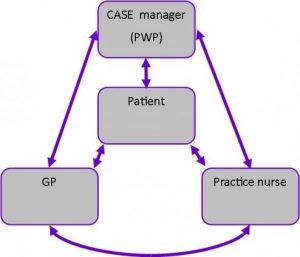
Illustration of the collaborative care model adopted in COINCIDE
-
- Key Elements
- Patients with PHQ depression score of ?10 referred to IAPT from trial manager;
- Biopsychosocial assessment using ABC model;
- Up to 8 sessions of brief psychological interventions based on CBT;
- Session 2 and 8 to be held jointly with practice nurse and PWP;
- Supervision as usual within IAPT;
- Stepped up or signposted to alternative services if appropriate.
Patients in the collaborative care arm received interventions modelled on those already given by IAPT but two sessions were designed to be shared between the patient, the nurse, and the PWP to aid integration. Collaborative care in COINCIDE was patient centred, involved a non-medical case manager and liaison between a GP and / or nurse.
Supporting Resources: Patient and Professional Manuals
Delivery of the treatment sessions in COINCIDE was supported by the use of patient and professional manuals. Instead of including the manuals used in the initial trial here, we are making the adapted versions of these available instead. Following the initial COINCIDE trial, the face-to-face training programme has been rolled out to a number of IAPT services, more information about which is available on the COINCIDE rollout page. As part of this rollout, and relying on the qualitative data from the initial COINCIDE trial, PPI consultation and close work with PWPs, the original manuals have been developed further.
- Patients with PHQ depression score of ?10 referred to IAPT from trial manager;

Trial Process and Participent Characteristics
Once GP surgeries agreed to be in the trial they were randomised to ‘collaborative care’ or ‘usual care’; the CONSORT flow diagram below shows the flow of participants through the trial after randomisation:
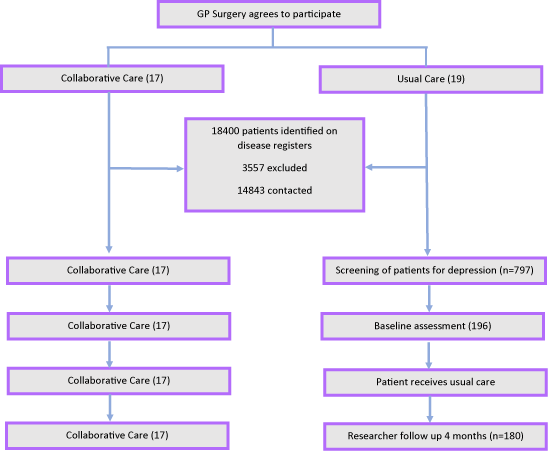
CONSORT flow diagram showing the number of patients recruited and followed-up at each stage of the trial
Participant characteristics
The participants in the trial were from deprived areas, had relatively high levels of depression – and many LTCs, but only half were treated for their depression or anxiety.
-
76% of participants were recruited from practices from moderately and heavily deprived areas;
-
Only 25% of participants were in paid employment;
-
63% of participants met criteria for moderately severe (or severe depression);
-
75% of participants met criteria for case-ness for anxiety;
-
Participants had a mean of 6.2 long term conditions in addition to either diabetes or coronary heart disease;
-
62% of participants were male, with a mean age of 58.5 years (11.7);
-
Half of participants were prescribed anti-depressant or anti-anxiety medication at baseline.
Therefore, participants in the COINCIDE trial had high levels of psychological and physical ill health and were mainly from deprived areas.
Key Findings from the Trial
There were a range of key findings in the COINCIDE trail from clinical findings and process outcomes to process of care and identification of strengths and weaknesses. Click on each of the links below to find out more:
- Clinical Findings
-
Mean scores were 0.23 SCL-D13 points lower (95% CI -0.41 to -0.05) in the collaborative care arm – equal to an adjusted standardised effect size of 0.30;
-
Improved anxiety outcome – equal to a reduction of 1.45 points on the GAD-7.
-
- Process Outcomes
-
Better self-managers on 5 of 8 domains of the Health Education Impact Questionnaire (heiq);
-
Rated care as more patient centred – congruent with goals of chronic care model;
-
More satisfied with their care;
-
No significant differences for Quality of Life (QOL), disease specific QOL, self-efficacy, disability, and social support.
Patients who received collaborative care were less depressed and anxious than those who received usual care; they were also more satisfied with their care, were better self-managers, and thought their care was more patient-centred.
-
- Process of care
While patients only received on average of four rather than eight sessions, at least half of patients had at least one joint treatment session with their nurse and PWP.
-
Patients with PHQ depression score of ≥10 referred to IAPT from trial manager;
-
Patients received a mean of 4.4 sessions (3.3, 0-14);
-
50 (26%) participants attended one joint integrated care session, and 46 (24%) patients attended two joint integrated care sessions;
-
Mean length of mental health treatment sessions was 27 mins;
-
Mean length of integrated care sessions was 19.7 mins;
-
Small but non-significant increase in antidepressant use during the trial (6% increase in collaborative care, 7% in usual care).
-
- Strengths and weaknesses
As with all trials, COINCIDE has strengths and weaknesses; some of these relate to the design of the trial and others relate to the implementation and impact of the intervention.
-
Strengths
-
Pragmatic design in routine settings;
-
Population had mental-physical multi-morbidity and from deprived areas;
-
Trained existing care providers to adopt collaborative care.
-
-
Weaknesses
-
Effect size less than the pre-specified effect;
-
Short term follow-up;
-
Only half of patient engaged with integrated care sessions.
-
COINCIDE included many patients that ordinarily would be excluded from trials but the overall effects were fairly modest and less than anticipated.
Read this BMJ editorial paper to learn more about the strengths and limitations of the COINCE care model.
-
- Key findings and implications
-
Integrated collaborative care can reduce depression and improve chronic disease self-management in people with mental-physical multi-morbidity;
-
Mental health providers and practice nurses can be trained to deliver patient centred integrated health care for people with mental-physical multi-morbidity;
-
COINCIDE can be potentially implemented within the context of routine chronic disease management with only minimal changes to the organisation of primary care.
The findings support the use of collaborative care for managing mental-physical multi-morbidity.
-
Local and national impact of the work
- The COINCIDE trail has been included in the 2016 multi-morbidity Cochrane review; it is the only UK based trial to have been included
- The COINCIDE model has also been referenced as an exemplar of good practice in the 2016 The Kings Fund report on ‘bringing together physical health and mental health’
- The training programme has been rolled out as part of the ENHANCE long term conditions study, funded by NIHR CLAHRC West Midlands,. As part of this training was delivered to 50 Psychological Wellbeing Practitioners (PWPs) from two IAPT teams.
- The training manuals have been endorsed by Health Eduation England as traning materials for IAPT professionals, this information can be accessed from here
- Face-to face training, utilising the COINCIDE model has been rolled out to over 20 different IAPT services thoughout England and Scotland.
- Named 2016 research paper of the year by the Royal Collage of General Practitioners.
Downloadable resources
- Training Manuals
- Blogspot
Integrating physical and mental healthcare in primary care for people with multimorbidity - Peter Coventry (February 2015)
Professor Karina Lovell blogs about our mental health work - Karina Lovell (October 2014)
- Publications
- Presentation
- Posters
Who did we work with
South Stafford and Shropshire NHS Foundation Trust
More information
For further information about the project, please contact Michael Spence (Programme Manager).