COVID-19: Health and Care Inequalities in the North of England
The North of England has consistently higher levels of poverty, poorer health outcomes, and worse social determinants of health than the rest of England.
We wanted to understand the impact of the COVID-19 pandemic and associated control measures on the health and productivity of the people of the North compared with the rest of England.
Our research provides compelling evidence that people in the North were more likely to die from COVID-19; were made poorer and endured a larger mental health impact. This information has been presented to government to inform strategy aimed at levelling up health and care inequalities.
In collaboration with the Northern Health Science Alliance (NHSA) and northern ARCs (North West Coast; Yorkshire and Humber; North East and North Cumbria), we have been involved in research looking at how COVID-19 has affected the North of England relative to the rest.
The report: "Child of the North: Building a fairer future after COVID-19"makes clear recommendations to policymakers about tackling the effects of the pandemic in the North, and addressing the underlying problems that already existed.
It highlights that during the COVID-19 pandemic, children living in the North of England:
- faced worse health and education outcomes than those in the rest of the country;
- missed more school, with estimated negative impacts on lifetime earnings;
- reported higher levels of loneliness and poor mental health; and
- faced higher levels of both relative and absolute poverty due to illness, long-COVID, and job loss.
Key findings and recommendations are here.
What has changed as a result of our research?
The emphasis on regional health inequalities in the Levelling Up White Paper brings some hope that there will be targeted action with the aim of better health outcomes for people living in the most deprived communities, including in the North of England.
There is a commitment in the White Paper to increase healthy life expectancy by five years by 2035 and to narrow the gap between local areas where it is highest and lowest by 2030.
All three reports have been shared widely with NHSA contacts within Government, including all northern MPs and representatives from relevant committees and All Party Parliamentary Groups, continuing to highlight the widening inequalities faced by people in the North that need to be addressed by Government, the Department of Health and Social Care and local policy makers.
Findings have also been shared and discussed with key policymakers from the Greater Manchester Health and Social Care Partnership and the Greater Manchester Combined Authority, which make up the newly formed NHS Greater Manchester Integrated Care System (ICS), as part of regular quarterly meetings.
Dr Luke Munford (Deputy Lead for the NIHR ARC-GM Economic Sustainability research theme) has presented findings and key recommendations from the reports to a range of policymakers, health and care professionals, and public and community groups. Key meetings/workshops/events include:
- Treasury Select Committee evidence session on “The Economic Impact of Coronavirus” - October 2020
- Manchester Academic Health Science Centre (MAHSC) seminar series, presented on "Inequalities during COVID-19: focussing on Greater Manchester & the North of England" (Sep 2021), attended by clinical academics and NHS trust representatives.
- The Centre for Urban Wellbeing, presented on "Mental health and wellbeing ‘poverty’ in England: concepts and the unequal spread" (October 2021)
- Addressing Health Inequalities through applied research in Greater Manchester (March 2022) to the voluntary sector and the public. Presentation here.
- Address by Prof Kate Pickett (NIHR ARC Yorkshire and Humber) at the All-Party Parliamentary Group on a Fit and Healthy Childhood (January 2022), about the "Child of The North: Building a fairer future after COVID-19’ report.
- As part of the Westminster Hall Debate on Regional Inequalities: Child Poverty (Volume 709; 2 March 2022); Liz Twist (MP for Blaydon) discussed the "Child of the North; Building a fairer future after COVID-19" report. Following this, the team were joined by parliamentarians, academics, charities, young people, organisations and civil servants at the parliamentary launch of the report in Westminster, alongside the NHSA, N8 Research Partnership and Northern ARC colleagues.
This has resulted in Dr Luke Munford being asked to be a member of the Manchester Marmot Health Inequalities Task Group.
Prof. Matt Sutton (Lead for the NIHR ARC-GM Economic Sustaunability research theme) sitting on the Greater Manchester Population Health Board to assist with discussions about how we feed into the development and thinking about inequalities in the NHS Greater Manchester Integrated Care System's 5-year plan.
Next steps
Following on from this work, we have obtained over £1m of additional external research funding to further explore, understanding and look at ways of addressing the health and care inequalities experienced, particulalry in the north of England:
Key resources and links
- Reports
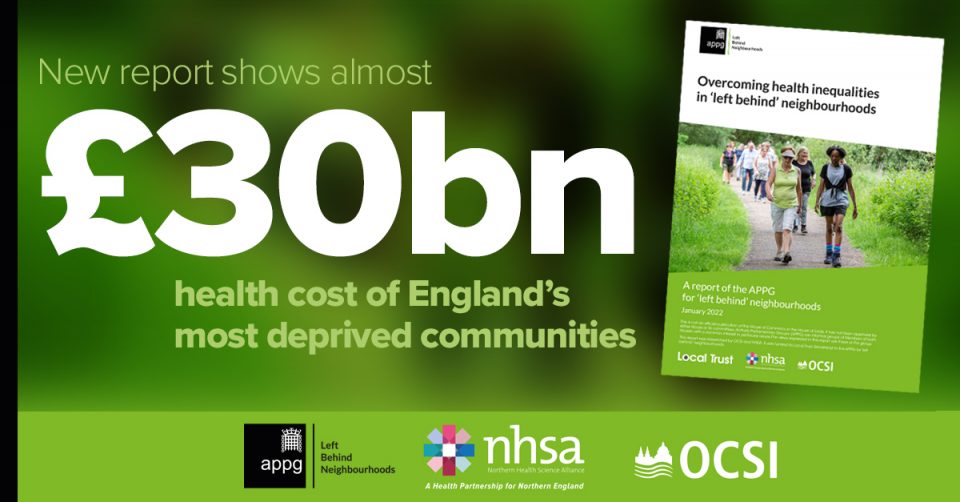
- Munford, Mott et al. (2022). Overcoming health inequalities in ‘left behind’ neighbourhoods. Northern Health Science Alliance and the APPG for ‘left behind’ neighbourhoods.
- Pickett K., Taylor-Robinson D., et al (2021) The Child of the North: Building a fairer future after COVID-19, the Northern Health Science Alliance and N8 Research Partnership.
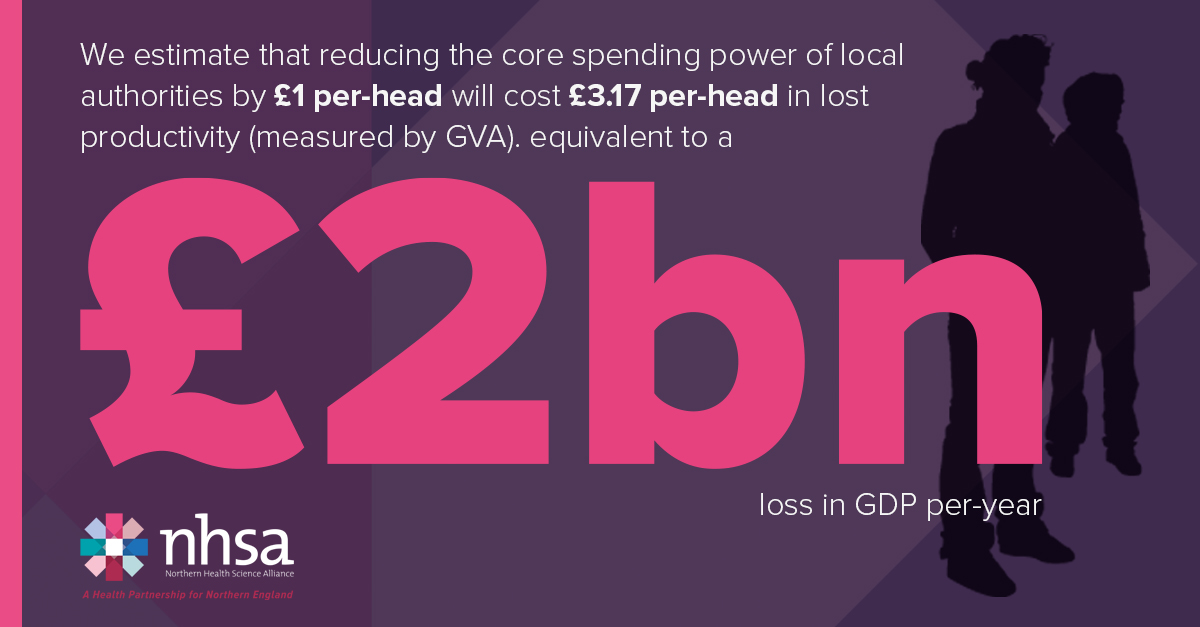
- Munford, L., Khavandi, S., et al, (2021). A year of COVID-19 in the North: Regional inequalities in health and economic outcomes, Northern Health Science Alliance, Newcastle.
- News stories
- Blogs